During this coronavirus pandemic, scores of the dead are coming from nursing homes and rehabilitation centers.
While it is understandable that the elderly by nature of their age likely had pre-existing conditions, there have been longstanding issues regarding notification of family, personal protective equipment (PPE) for workers and communication with government.
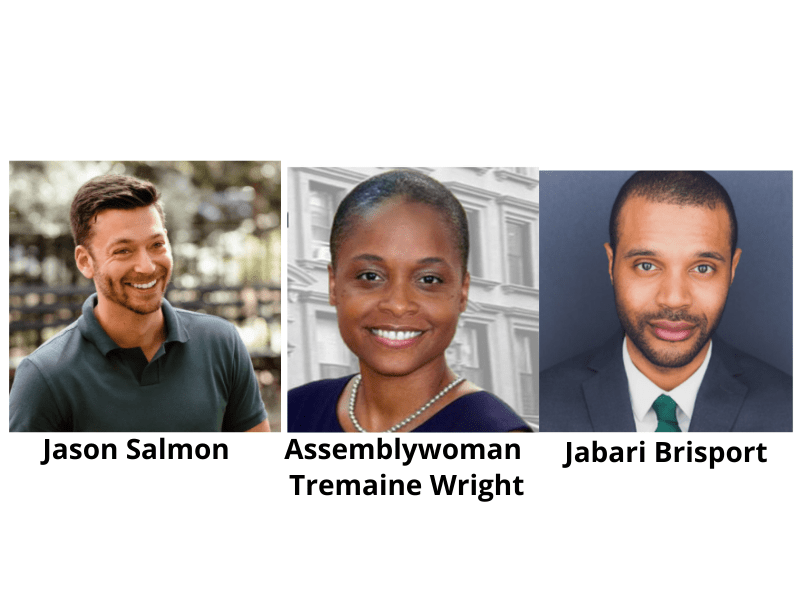
Thus KCP put the following question to the three candidates Assemblymember Tremaine Wright, Jason Salmon and Jabari Brisport running in the upcoming 25th Senate District Democratic Primary on June 23. The district includes Fort Greene, Boerum Hill, Red Hook, Bedford-Stuyvesant, Sunset Park, Gowanus, and Park Slope.
Given that the NY State Department of Health is the regulatory government body overseeing all nursing homes, what kind of legislation and/or measures concerning nursing homes would you advocate for as a state assembly or senate member?

Tremaine Wright: “I believe there are a number of immediate administrative /policy changes that would prove to be helpful in the management of our nursing homes.
“Our nursing homes are privately owned and operated entities. Like many businesses they were not prepared for a pandemic. In this instance, we found nursing homes suffering from a lack of information about this virus. They too were relying on briefings to determine the right approach and necessary steps. But the lack of information meant nursing home staff was caring for patients who were positive for COVID-19 but never identified.
“The result was that in addition to a growing number of sick residents many of the staff became ill themselves and had to call out. This first came to my attention when I learned that nursing homes were not accepting their residents back when the resident was discharged from the hospital after being treated for COVID-19. Like many, I initially thought the nursing home was simply refusing the to admit the resident because they had tested positive for the virus . But I would later learn that the nursing home was actually prohibited from accepting the returning resident because they did not have enough staff. The staff to patient ratios would have been too low if the resident was re-admitted. So, residents remained in the hospital instead of returning to the homes.
“This staffing problem diminishes the quality of patient care, exposes staff to more risk, increases healthcare costs, and multiplies stress levels for family and loved ones.
“To help correct this problem Nursing Homes must be connected to the larger health care system in a more concrete manner. We should support policy that promotes: Formalizing relationships between nursing homes and area hospitals; Increasing the number of Health Aids, Certified Nursing Assistants, and Nurses; and Connecting Nursing Homes with trained personnel.
“These policy proposals would shift our nursing homes from isolated entities to full participants in a supportive network of information, supplies and employee talent. We would be better able to provide nursing home residents with acute care and testing. We would have better information to share with family members on the care and location of loved ones.
“Once connected to the healthcare network, our nursing homes can avail themselves of better supply chains, medical processes and information sharing. Part of the challenge for us during this healthcare emergency was that individual nursing homes did not have capacity to respond in real-time to the demand. Networking support will give nursing homes flexibility. Additionally, policy that supports educational pipelines into the healthcare profession will be beneficial all around and meet the growing demand in our state. As we have seen over the last few weeks it was difficult for nursing homes to operate because of staffing shortages. So while we grow the profession we must also have a system in place that supports the emergency needs of nursing homes to be properly staffed at all time.”

Jason Salmon: “COVID has exposed the inequities in our healthcare system. For years we have required nurses to put their lives at risk and provide quality healthcare services with little to no support. We know that nurse-to-patient ratios have been a driver for adverse patient outcomes, poor-quality healthcare, and high death rates, yet our representatives have continued to cut hospital funding and have required nurses to care for upwards of 10 patients at a time. This is particularly true for nursing homes in communities of color where underpaid and under-appreciated Black and Brown women make up the majority of essential workers.
“By understaffing our hospitals we are putting our patients and community at risk. We must implement nurse-to-patient ratios and provide our hospitals with the PPE they need so together we can flatten the curve.”

Jabari Brisport: “Our nursing homes and rehabilitation centers are underfunded, just like the rest of our healthcare industry. Nursing home budgets were temporarily on the chopping block this past legislative session, with $123 million in anticipated cuts, but thankfully those cuts have been avoided (unlike the deeply unfortunate cuts to Medicaid). When our nursing homes are underfunded, it means that they become understaffed and under-resourced. That’s why this campaign is advocating that we implement the NY Health Act, a single payer healthcare system for New York that also includes provisions to fund long term care (nursing homes and rehabilitation centers.”