Sherry Tucker is CEO of WellLife Network, one of New York’s largest health and human services organizations. She oversees more than 1,500 employees, serving over 25,000 individuals annually. She has led WellLife through significant expansions, financial stabilization, and program enhancements. Sherry has also been deeply involved in civic and philanthropic work. She founded the Giving Hope through Faith Foundation, which raised over $1 million to support families affected by pediatric cancer.

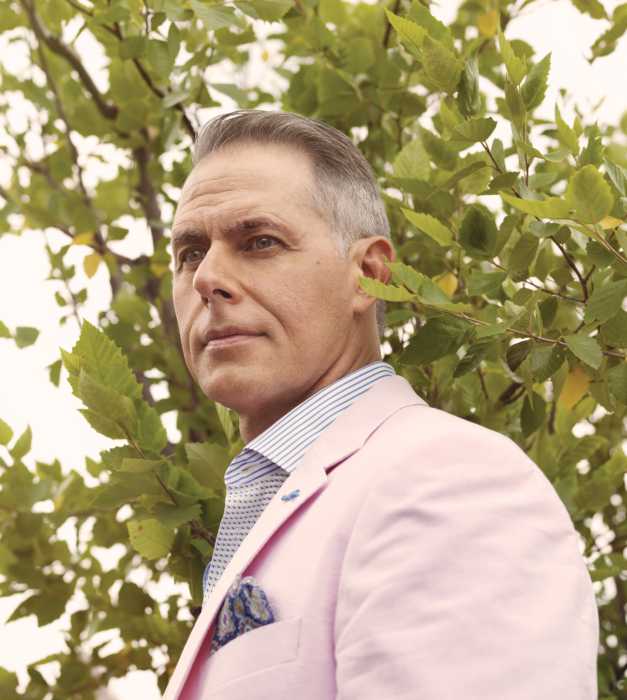
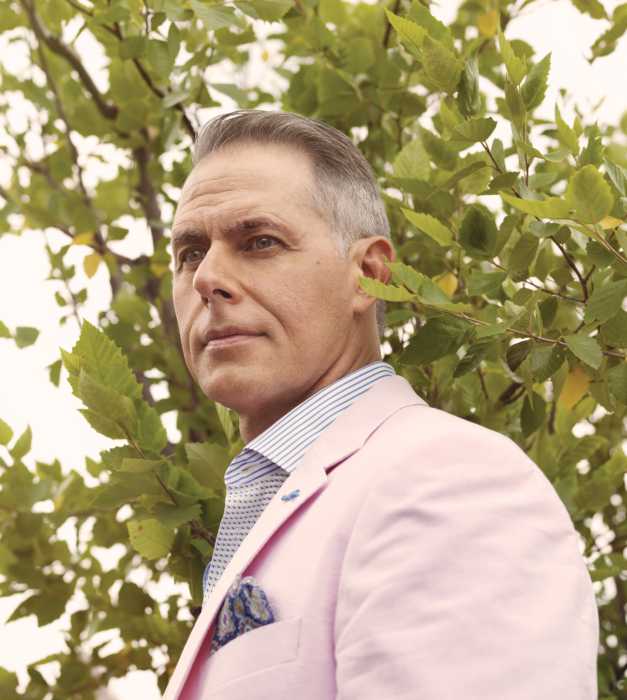
David Wagner
President and CEO, MJHS Health System | President, Elderplan/HomeFirst

David Wagner is president and CEO of MJHS Health System and president of Elderplan/HomeFirst. He leads the premier not-for-profit organization, which includes home care, hospice and palliative care, two centers for rehabilitation and nursing care, an institute for innovation, and Elderplan/HomeFirst health plans. He is a driving force behind advances in health care innovation, quality care, financial reporting and revenue, as well as relationship-building with state workgroups, governmental agencies and national regulatory organizations.
How do you expect the health care field to change in the next five years?
The health care field will undergo rapid transformation, driven by digital innovation and industry consolidation. AI and digital tools, like predictive modeling, will identify at-risk members and support earlier and new forms of intervention. While our clinical teams will remain central to the delivery of member-centered, quality outcomes, data-driven insights and integrated systems will support delivery of even more personalized and accessible care for more members. Mergers and acquisitions will also continue to reshape our landscape.
As this year comes to an end, what are your goals for 2026?
My primary goal for 2026 is to complete the groundbreaking merger and lead subsequent integration of Elderplan/HomeFirst and VillageCareMAX under a new brand name. Bringing together two mission-driven, not-for-profit equals under one plan – serving nearly 100,000 members – will give us the scale necessary to enhance investment in member care, provide resilience amid a changing health care landscape, support future growth, and advance our shared commitment to the people and communities we both currently serve.

Pat Wang
President and CEO, Healthfirst

Pat Wang joined Healthfirst as president and CEO in 2008. She feels lucky to have been raised by her immigrant parents who instilled the values of hard work, gratitude, and never giving up. Healthfirst today proudly serves more than 2 million members with some of the highest quality health insurance products in the state and nation and through the lens that all health care is local.

Eric Wei
CEO, NYC Health + Hospitals | Bellevue

Dr. Eric Wei is CEO for NYC Health + Hospitals/Bellevue, the oldest hospital in the United States, dating back to 1736. A practicing emergency medicine physician, he also serves as senior VP for NYC Health + Hospitals, caring for over 1.3 million New Yorkers annually. He is a professor of emergency medicine at the Icahn School of Medicine at Mt. Sinai and adjunct professor at the Columbia University Mailman School of Public Health.
Doug Wirth
President and CEO, Amida Care
Since 2006, Doug Wirth has served as president and CEO of Amida Care, a Medicaid Special Needs Health Plan (SNP) in NYC. Under his tenure, Amida Care’s successful care model, designed to deliver specialized care to people needing intensive services, has empowered thousands of New Yorkers affected by HIV to take control of their health and get about the business of living their lives. Amida Care has grown to become the largest SNP in New York.
What piece of health care related legislation would you like to see passed in the near future?
Implementation of the NY legislature’s actions to protect providers of gender-affirming care (GAC), including expanding NY’s Shield Law to shield providers and patients from legal action originating in other states. NY-only funding for a GAC Fund to increase access, passing legislation to prohibit insurers from taking adverse action against providers for offering GAC. We need HR1’s repeal or reform. HR1 would cause 1.5M NYers to lose coverage and NY to lose $13.5B in health care funding.
How do you expect the health care field to change in the next five years?
I remain hopeful that there will be bipartisan support to ensure health care is delivered to all U.S. residents through multifaceted approaches and diverse payment strategies. New York State would lose $13.5B in health care funding and 65,000 jobs due to Medicaid cuts. If we advocate with care and compassion, I am confident elected leaders will understand that equal access to health care is a fundamental right – and good for the economy.
As this year comes to an end, what are your goals for 2026?
Expand the impact of HIV SNPs to increase PrEP access amongst NYers with Medicaid at greatest HIV risk. Create a public-private partnership (NYSDOH/Pharma) to make game-changing Long-Acting Injectable HIV treatment and prevention readily available to end the HIV epidemic. I would like to be part of a coalition movement focused on public accountability, across the political spectrum, for protecting insurance coverage, while also improving the country’s health care delivery and safeguarding the health care safety net.

Jameela Yusuff
Senior Vice President and Chief Medical Officer, Episcopal Health Services

Dr. Jameela Yusuff, SVP and chief medical officer at EHS, drives clinical strategy, quality improvement, and service expansion across the system. With 20+ years of leadership experience, she previously served as chief medical officer at University Hospital of Brooklyn and Medical Director of the STAR Program. Board-certified in internal medicine, infectious diseases, and addiction medicine, she holds an M.D., MPH, and M.S. in health care delivery leadership and serves on national and local medical boards.
What piece of health care related legislation would you like to see passed in the near future?
A priority should be national legislation mandating universal interoperability across all electronic health record (EHR) systems. This would eliminate data silos, enable seamless information exchange between different health care systems, reduce administrative waste, and directly improve patient safety by ensuring complete medical histories are available at the point of care.
How do you expect the health care field to change in the next five years?
In the next five years, we will see greater use of AI for diagnostics and administrative efficiency, addressing staff burnout, and improving patient access, particularly in primary care and behavioral health. However, the industry will also face challenges, including cybersecurity risks and the need for new regulations to keep pace with technological changes. Additionally, the industry will need to develop innovative approaches to address the increasing staffing shortages that are expected.
As this year comes to an end, what are your goals for 2026?
My goals for 2026 include prioritizing cost management amid rising expenses, leveraging artificial intelligence for operational efficiency and better diagnostics, and improving access to care. Other areas of focus are enhancing the patient and team member experience, optimizing clinical outcomes through data analytics, and addressing ongoing staffing shortages.

Michelle Zettergren
Chief Sales and Marketing Officer and President of Labor, Brighton Health Plan Solutions

As the first female president of labor and chief sales and marketing officer of Brighton Health Plan Solutions (BHPS), Michelle Zettergren brings over 25 years of experience in the health insurance industry, leading the charge to transform how health care is accessed and delivered. Michelle’s unique leadership and forward-thinking approach have allowed BHPS to set the standard for health care enablement, providing innovative, customizable solutions that achieve better health outcomes at lower costs.
What piece of health care related legislation would you like to see passed in the near future?
The 2025 Budget Reconciliation Act – which includes over $1 trillion in cuts through 2034 and restricts eligibility for Medicaid, Medicare and Affordable Care Act plans – could result in a massive hit to our social safety net. It could leave 15 million more people uninsured and increase health care costs for all Americans. I’m hopeful for revisions that protect the most vulnerable and stabilize the commercial market from the effects of uncompensated care and lost provider access.
How do you expect the health care field to change in the next five years?
We can expect the health care landscape to shift toward more integrated care delivery, focusing on centers of excellence and unique provider contracts that improve patient outcomes. I also anticipate workforce changes that drive greater demand for virtual and technology-forward care and solutions. Increased use of AI across health care will likely improve medical interventions and payer integrity. Finally, we can expect to see a greater level of cost transparency for health plans and their members.
As this year comes to an end, what are your goals for 2026?
As we approach 2026, the market is seeing significant increases in medical costs. We are focusing on partnering with our clients on custom solutions such as point solutions, tailored medical interventions, redirection of care and unique provider contracting approaches that can help manage spending and improve access and quality of care for members. We’re also continuing to invest in technology advancements and AI tools to support our clients’ benefit plans and member experience.





