Two New York City-based doctors and David Prize finalists hosted a zoom meeting discussing healthcare inequity and training of front-line workers in dealing with patients that have been exposed to trauma – and often repeatedly so.

Many healthcare systems perpetuate economic and health inequities that stem from systemic racism, according to Dr. Suzette Brown, Queens pediatrician and co-founder of Strong Children Wellness (SCW). These inequities and the improper training of front-line workers to respond to traumatic situations can further compound traumas, which has been highlighted by the recent COVID-19 pandemic and Black Lives Matter protests.
The Defund the Police movement, for example, which has resulted from Black Lives Matter protests, stresses how police improperly respond to traumatic situations, and that funding should be reallocated to communities of color.
“Shifting resources away from law enforcement for things that law enforcement shouldn’t be the first responders to I think is a really important conversation to have,” says Brown, citing that police are often the first to respond to domestic violence and mental health calls, but that communities may be better equipped to handle such situations.
“How you’re treated by law enforcement and medical professionals is traumatic by itself,” agrees Dr. Robert Gore, a Brooklyn-based emergency physician.
As more and more front-line workers work in spaces where trauma is unavoidable, they need to be trained in handling an array of stress factors, including but not limited to gun violence, COVID-19, police brutality, heart disease, or a combination of these factors.

“We’ve had many patients who have been impacted by all of those things, not just isolated incidents,” says Gore. “Front line workers need to receive the same sort of informed care and resources that we provide for our patients.”
Just like Brown, Gore also emphasizes the importance of community support, which may be more effective in dealing with the root causes of trauma.
In his years of practice, Gore has noticed a disconnect between healthcare workers and patients, who often have an “us vs. them” mindset. This adversely affects the patient’s ability to heal from traumas. When people don’t have access to good healthcare, they come back,” says Gore.
As an example of how community support can improve healthcare, Gore founded Kings Against Violence Initiative to address the reoccurring violence that disproportionately affects young people of color and leads to repeated injuries, trauma, and even death. He stresses that prevention is not only cheaper than treating someone, but can also be life-saving, and that violence should be seen as a form of disease due to the resulting injuries.
SCW, on the other hand, has begun to offer virtual consultations to families in order to bridge gaps in providing healthcare to all patients, which has become more challenging during the COVID-19 crisis. As a result, the Queens-based organization now receives patients from around and even outside the city.
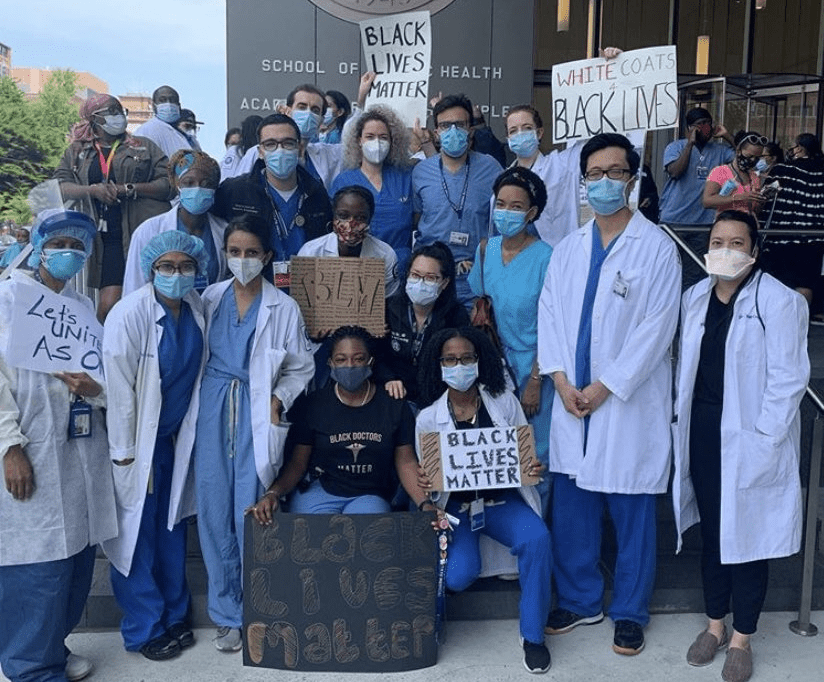
To further address racial inequities in trauma and public health issues, Brown and Gore encourage physicians to join the physical anti-racism network, which tackles issues relating to criminal justice reform, health, housing, and education.
Furthermore, trained physicians can join the #WhiteCoats4BlackLives movement and provide health services at protests, ensuring that those at the front lines of trauma are receiving the care they need.
“The goal of any health care practitioner is to become obsolete,” says Gore. “Checkups are one thing. But going back there for ongoing treatments for something that is preventable is a problem in and of itself.”