CDC Guidelines on How to Integrate Back After Recovery
The CDC issued new guidelines this week on how to proceed after you have recovered from coronavirus.
If you are symptomatic and have a confirmed or highly suspected case of COVID-19, the federal agency advised waiting 10 days since symptoms first appeared, including three days with no fever, before seeing others. Overall symptoms must also have improved before coming out of isolation.
“Depending on your health care provider’s advice and availability of testing, you might get tested to see if you still have COVID-19. If you will be tested, you can be around others when you have no fever, symptoms have improved, and you receive two negative test results in a row, at least 24 hours apart,” the CDC said.
If you have tested positive for COVID-19 and are not showing symptoms, the CDC also advised waiting 10 days from the time you were tested before having contact with other people. Asymptomatic people must continue to be asymptomatic within that period of time.
But the moment someone begins to develop symptoms, they are advised to follow the guidelines first written.
Those with weakened immune systems, such as those undergoing cancer treatment, should possibly wait longer than 10 days — but the federal agency advised that those patients speak to their health care provider for more personalized recommendations.
“It is important to remember that anyone who has close contact with someone with COVID-19 should stay home for 14 days after exposure based on the time it takes to develop illness,” the CDC added.
If you are wondering why there is a ten-day minimum, it’s because of two studies in its memo titled: “Symptom-Based Strategy to Discontinue Isolation for Persons with COVID-19.” The studies referenced by the federal agency found that the “statistically estimated likelihood of recovering replication-competent virus approaches zero by 10 days.”
But there is a debate on if ten days is the right amount.
To read more on this, go to Foxnews.com
Fed Bipartisan Passage on Small Business Owners Spending Flexibility

The House of Representatives passed new legislation that gives small business owners more flexibility in how they spend money from in The Paycheck Protection Program.
The Paycheck Protection Program, one of the core parts of the $2 trillion pandemic rescue package passed in March, includes standards for how companies have to use their loans in order to get them forgiven. The measure passed Thursday would ease those rules.
The plan would reduce the share of aid money small business are required to spend on payroll from 75% to 60% (the PPP’s architects aimed to encourage companies to keep workers employed), extend the window businesses have to use the funds from two months to six months, push back a June 30 deadline to rehire workers, extend the time recipients have to repay the loan and let companies that get loan forgiveness defer payroll taxes.
It was passed nearly unanimously, but it’s held at the senate level as of late. The Senate will reconvene next week.
While this decision was bipartisan, the next phase of the relief package brings a struggle. Democrats would like to see more direct payments to individuals and to give relief to state and local governments while extending an enhanced federal unemployment insurance benefit. The GOP questions the need to spend more taxpayer money on recovery efforts, it has pushed for liability protections for businesses and doctors as most of the country restarts commerce.
To read more on this story, go to CNBC.com
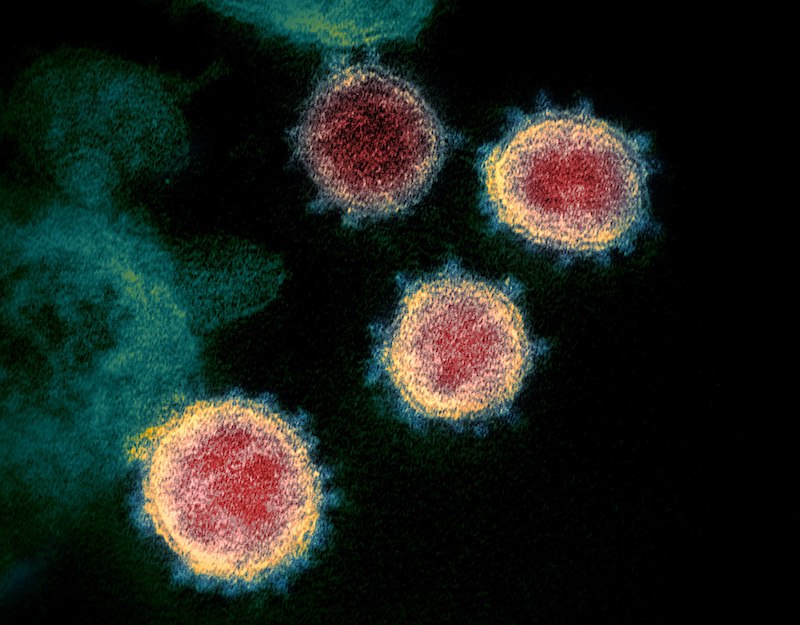
Debate Continues if COVID-19 Originated in Wet Markets?

According to medical experts at the Wuhan Institute of Virology (WIV) and U.S. based experts, the first case of SARS-CoV-2 didn’t emerge from a Wuhan wet market but rather the live animal market may have been the site of a superspreader event, where one person spread the virus to many other people.
The theory that the SARS-CoV-2 (the virus that causes COVID-19) jumped from animals to humans in Wuhan’s Huanan Seafood Wholesale Market has been discredited, and that the virus originated from somewhere else.
“I haven’t seen anything that makes me feel, as a researcher who studies zoonotic disease, that this market is a likely option,” said Colin Carlson, a professor at Georgetown University who studies the spread of such zoonotic viruses, which transmit between animals and humans. Carlson does not work for the WIV.
Although the theory of animal to human transmission was plausible, the animal host needs to come into contact with humans somewhere, he explained, and viruses often jump from one animal to another before breaking into the human population.
Scientists found that the genome of SARS-CoV-2 was closely related to coronaviruses isolated from horseshoe bats in China. From there, scientists suspect the virus may have jumped to another animal and then hopped to humans in the wet markets.
A number of early cases of the outbreak in Wuhan were tied to the Huanan Seafood Wholesale Market. Later, researchers took environmental samples that suggested the virus had landed on surfaces in the market. But in the period since, tissue samples from the market’s animals have revealed no trace of the virus. For the virus to jump from animals to humans, the animals have to actually be carrying it.
“None of the animals tested positive. So since January, this has not actually been particularly conclusive. But this has developed into a narrative,” he said.
Carlson said his colleagues in China have been careful and precise in their work, publishing data according to international regulations that any scientist anywhere in the world can examine, and that strongly supports the conclusion that the Huanan Seafood Wholesale Market wasn’t the source of the virus.
To read more on this, go to LiveScience.com
Blood Clots a Revealing Factor in COVID-19
Findings in the Lancet Respiratory Medicine showed autopsies of 10 African-American COVID-19 victims with their lungs clogged with blood clots, and it may help to understand why blacks are suffering so much more from Covid-19 in the U.S. and in some other countries such as Britain, the researchers said.
All 10 patients had underlying conditions that have been shown to worsen the infection, including high blood pressure, diabetes and obesity. But genetic factors could also be at play, the team at LSU Health New Orleans School of Medicine said.
“We found that the small vessels and capillaries in the lungs were obstructed by blood clots and associated hemorrhage that significantly contributed to decompensation and death in these patients,” Dr. Richard Vander Heide, head of pathology at the medical school, said in a statement.
The doctors found blood markers called D-dimers, which are signs the body has been working to break down blood clots. “I think obesity is important in our population,” Vander Heide told CNN.
Fat tissue activates inflammatory chemicals — one of the mechanisms that underlies obesity’s link to a variety of diseases. Covid-19 infection generates even more inflammation, which doctors believe is involved in the damage caused by Covid-19 and, perhaps, the generation of blood clots.
It is a common report from doctors all over the U.S., that their patients’ bodies have been riddled with blood clots. Some early studies have shown that treating patients with anticoagulants can help.
“One of the things people are seeing with COVID now is the cytokine storm that is generated by the virus,” Vander Heide said. The cytokine storm is the flood of inflammatory immune system compounds some people produce in response to the infection. “We can see it in our sections of the lungs. We see the viral effects in the cells,” he added.
The findings may shed light on why blacks, in general, are suffering more from Covid-19 in the UK, Dennis McGonagle of the University of Leeds and colleagues wrote in a linked commentary.
“A feature of the coronavirus disease 2019 pandemic has been increased mortality in Black, Asian, and Minority Ethnic groups in the UK, which has resulted in the UK Government setting up an emergency investigative task force,” they wrote.”In the USA, mortality from COVID-19 has been particularly high in African American communities in large cities.”
“Black patients had higher prevalence of obesity, diabetes, hypertension, and chronic kidney disease than white patients,” Dr. Eboni Price-Haywood and colleagues at Ochsner wrote.
But many factors likely underlie the racial discrepancies, they said.
To read more on this, go to CNN.com










