With death from drug overdoses expected to exceed 1,000 this year for the first time ever in the city, Gov. Andrew Cuomo announced today that new health insurance reforms to combat heroin and opioid abuse will take effect Jan. 1.
The state reforms, part of a legislative package that Cuomo signed earlier this year, will require health insurance plans to cover treatment services provided to New Yorkers suffering from opioid addiction, increase access to treatment, expand community prevention strategies, and limit the over-prescription of opioids in New York.

“With these landmark reforms fully enacted, we have removed artificial barriers that prevented New Yorkers from receiving the help they need and put into place new safeguards to get these drugs off the street,” said Cuomo. “As families and communities across the nation grapple with the devastating effects of this heroin and opioid crisis, New York is leading the fight to stamp out this disease once and for all.”
The new insurance-related protections are the final components of the package to take effect and include four measures to remove burdensome access barriers for inpatient treatment and medication. These measures:
· End Prior Insurance Authorization to Allow for Immediate Access to Inpatient Treatment as Long as Such Treatment is Needed: Insurers must cover necessary inpatient services for the treatment of substance use disorders for as long as an individual needs them. In addition, the legislation establishes that utilization review by insurers can begin only after the first 14 days of treatment, ensuring that every patient receives at least two weeks of uninterrupted care before the insurance company becomes involved.
· End Prior Insurance Authorization to Allow for Greater Access to Drug Treatment Medications: Insurers cannot require prior approval for emergency supplies of drug treatment medications. Similar provisions that also apply to managed care providers treating Medicaid recipients who seek access to buprenorphine and injectable naltrexone took effect in June.
· Require All Insurance Companies Use Objective State-Approved Criteria to Determine the Level of Care for Individuals Suffering from Substance Abuse: All insurers operating in New York State must use objective, state-approved criteria when making coverage determinations for all substance use disorder treatment in order to make sure individuals get the treatment they need.
· Mandate Insurance Coverage for Opioid Overdose-Reversal Medication: Insurance companies must cover the costs of naloxone when prescribed to a person who is addicted to opioids and to his/her family member/s on the same insurance plan.
 According to a story in today New York Times, a large majority of the overdoses are due to the drug, fentanyl, a synthetic opioid commonly used as an anesthetic for surgery and which can be 100 times more potent than morphine.
According to a story in today New York Times, a large majority of the overdoses are due to the drug, fentanyl, a synthetic opioid commonly used as an anesthetic for surgery and which can be 100 times more potent than morphine.
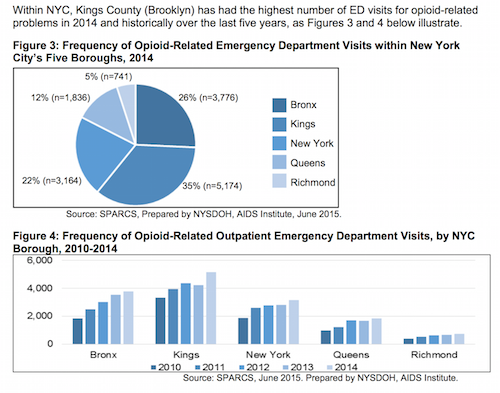
Brooklyn, according to a City Department of Health and Mental Hygiene Report, has had the most opioiod-related hospital emergency room visits between 2010-2014 in the state.
The package’s other provisions already in effect include:
ENHANCING ADDICTION TREATMENT SERVICES
· Increasing Evaluation for Individuals Incapacitated by Drugs from 48 to 72-Hours: Families can now seek 72-hours of emergency treatment, an increase from 48-hours, for their loved one so that they can be stabilized and connected to longer-term addiction treatment options while also balancing individual rights of the incapacitated individuals.
· Requiring Hospitals to Provide Follow-Up Treatment Service Options to Individuals Upon Hospital Discharge: Hospital medical staff must provide discharge-planning services to connect patients who have or are at-risk for substance use disorder with nearby treatment options to provide continuous medical care.
· Allowing More Trained Professionals to Administer Life-Saving Overdose-Reversal Medication: Trained professionals can now administer naloxone in emergency situations without risk to their professional license.
· Expanding Wraparound Services to Support Long-Term Recovery: The wraparound program launched in 2014 to provide services is now expanded to individuals completing treatment including education and employment resources; legal services; social services; transportation assistance, childcare services; and peer support groups.
STRENGTHENING COMMUNITY PREVENTION STRATEGIES
· Reducing Prescription Limits for Opioids from 30-days to Seven Days: The limit for initial opioid prescriptions for acute pain has been reduced from 30-days to no more than a 7-day supply, with exceptions for chronic pain and other conditions.
· Requiring Ongoing Education on Addiction & Pain Management for All Physicians and Prescribers: Health care professionals must complete three hours of education every three years on addiction, pain management, and palliative care.
· Mandating Pharmacists Provide Easy to Understand Information on Risks Associated with Drug Addiction and Abuse: Pharmacists must provide educational materials to consumers about the risk of addiction, including information about local treatment services.
· Requiring Data Collection on Overdoses and Prescriptions to Assist the State in Providing Additional Protections to Combat this Epidemic: The State Commissioner of Health must report county-level data on opioid overdoses and usage of overdose-reversal medication on a quarterly basis.
Consumers with questions about the new insurance-related consumer protections are urged to contact DFS at the agency’s toll-free hotline at (800) 342-3736 or at www.dfs.gov.










